The Coronavirus, Trauma, and PTSD
The coronavirus, trauma, and PTSD have become an unholy trio in recent months. June is PTSD Awareness Month, and to mark the occasion this post highlights preventative tools parents can use with children. This excerpt from my book, Does My Child Have PTSD? What To Do When Your Child Is Hurting from the Inside Out), explains how parents can help kids process trauma so it doesn’t become PTSD.
Parents can practice proactive measures to help their children process traumatic events and thus prevent PTSD. In Trauma-Proofing Your Kids: A Parent’s Guide for Instilling Confidence and Resilience, Dr. Peter Levine and Maggie Kline promote a step-by-step process they call “first aid for trauma prevention.” They suggest following these steps after a child has experienced a traumatic event.
- Check your own body sensations first. Children are very sensitive to the emotional states of adults. Parents or other caring adults must compose and calm themselves before attempting to calm a child.
- Assess the situation. Look for signs of shock in the child, and if you see them, have the child sit with you until the shock wears off.
- As the shock wears off, guide the child’s attention to his body sensations. Ask increasingly specific questions about how the child feels in his body to guide him back to the present.
- Slow down and follow your child’s pace by careful observation of changes. Leave time between questions for the child to resolve each cycle of emotions, and be alert to cues that indicate a cycle is complete.
- Keep validating your child’s physical responses. If your child is trembling or crying, put a hand on his shoulder and tell him it’s okay to let the scary stuff out.
- Trust in your child’s innate ability to heal. This gets easier as you practice the steps of trauma first aid. Remember not to rush the process, and give your child the necessary time to process excess energy and expel it.
- Encourage your child to rest, even if he doesn’t want to. Dr. Levine and Kline believe that sleep helps a child process the event and discharge energy. By providing a calm, quiet environment, you help your child complete the healing.
- Attend to your child’s emotional responses and help make sense of what happened. This step comes later, after the child is once again calm and rested. Set aside time to ask the child what happened. Give reassurance that it’s okay to feel scared, sad, guilty, or embarrassed. Share a story about a time when you felt like your child feels. Assure your child of your unconditional love. Give your child time to retell the story using drawing, clay, or play.
When our son was four, he needed one final corrective surgery on his esophagus and stomach. Many, many years later he told me, “When they took me into the operating room, it was so scary. They wheeled me in on a hard bed. The operating room was icy cold. The walls were glaring white, and the lights were so bright they hurt my eyes. Then these people without any faces leaned over and told me everything was okay. But it wasn’t okay. It was terrible. And I went crazy, trying to get off the table and flailing my arms until those people without faces pinned me to the table.”
His words perfectly described what masked OR nurses must have looked like to him—people without faces. His recounting also reminded me of what a nurse said after our little boy arrived in the pediatric intensive care unit. “He went crazy.” She sounded none too pleased. “He pulled all the monitor wires and his IV.”
“Let me go in to him,” I said. “I’ll calm him down.”
“No,” she said firmly, “not until he’s settled down.”
I waited a long time, helpless and hurting, before they let me see him. If I had known then what I know now, I would have insisted on seeing him immediately. And if trauma first aid had been around back then, I would have used it to help him process what had happened to him.
Before entering his room, I would have taken some deep breaths to calm myself. Then I would have prayed for calm beyond what I could muster on my own. Once in the room, I would have taken time to study his face. Was it tear-streaked, pale, his expression pained? And then I’d have checked his body for signs of shock. Was his body rigid? Trembling? Was his breathing too fast, too, slow, or labored?
Having just endured several hours of major surgery, our little boy would be in shock. I would have offered the best first aid possible at that point—sitting beside his bed, holding his hand, stroking his forehead, rubbing his cheek, and giving constant reassurances of “Mommy’s with you, Allen,” interspersed with verses of his favorite lullabies.
Eventually, as the shock of the situation and the surgical pain eased, perhaps once he had moved to a regular room, I would have asked, “Allen, how does your tummy feel?”
“Hurts.”
“Does anything else hurt?”
“My foot.”
“Yes, the needle in your foot must hurt. Does your hand hurt, too?”
He would hold up his hand and look at it. “No. No owie on my hand.”
“Then can I hold your hand?”
Allen would nod, and I’d hold his hand. “Let’s pretend we’re holding a bunch of balloons together. Are you holding them tight?”
He would nod.
“Now, let’s pretend to put all the owies from your tummy and your foot inside the balloons.” I would wait a few seconds. “Did you do it?”
He’d nod again and smile a little.
“Okay, on the count of three, we’ll let go of the balloons and watch them carry your owies out the window and into the sky.”
He would smile again, and we’d look out the window, imagining the balloons disappearing in the bright blue Iowa sky. I would notice that his body would be more relaxed and his breathing would have calmed.
Over the next few days in the hospital, several times a day, I would have looked for signs of shock or pain returning. When it did, I would’ve repeated the questions about where he hurt and how, along with questions about what parts of his body didn’t hurt. Then I would have helped him focus his attention on where his body didn’t hurt, perhaps by playing clapping games or singing silly songs, along with hand motions.
And we could’ve made up stories—a favorite pastime for him—about one of his stuffed animals having a sore tummy after surgery. The story would have included the main character being frightened in the pediatric ICU and pulling at wires and needles. When Allen appeared scared by the story or trembled, I would have paused until his reaction, caused by the pent-up energy inside him, subsided. I would’ve reassured him, “Mommy’s here. I’ll stay right here until the scary feeling goes away.”
Had I known then what I know now, we would have repeated the stuffed-animal-has-surgery story for several days or weeks or however long it took until he could process all the trauma and dispel the energy trapped inside. Perhaps he would eventually have been able to further process the event by telling the story back to me in his own words.
Excerpted from Chapter 11 of Does My Child Have PTSD? Does My Child Have PTSD? What To Do When Your Child Is Hurting from the Inside Out (Familius, 2015)
Do you like what you see at DifferentDream.com? You can receive more great content by subscribing to the monthly Different Dream newsletter and signing up for the daily RSS feed delivered to your email inbox. You can sign up for the first in the pop up box and the second at the bottom of this page.
By Jolene
Related Posts
Educators Care about Traumatized Kids
This summer, I facilitated trauma training classes for more than 80 educators and realized something very heartening: educators care about traumatized kids.
The Hope Anew Disability Podcast
The Hope Anew Disability Podcast is the latest offering from Jonathan and Sarah McGuire. Learn who it’s for and what it’s about in this post.
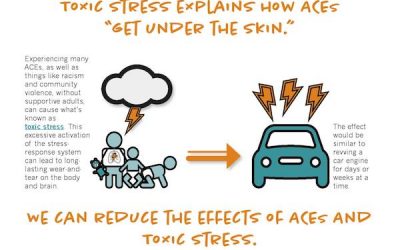
The ACEs and Toxic Stress: Implications for Children with Special Needs?
This infographic shows the relationship between ACEs and toxic stress. This relationship has implications for our children with special needs.





0 Comments